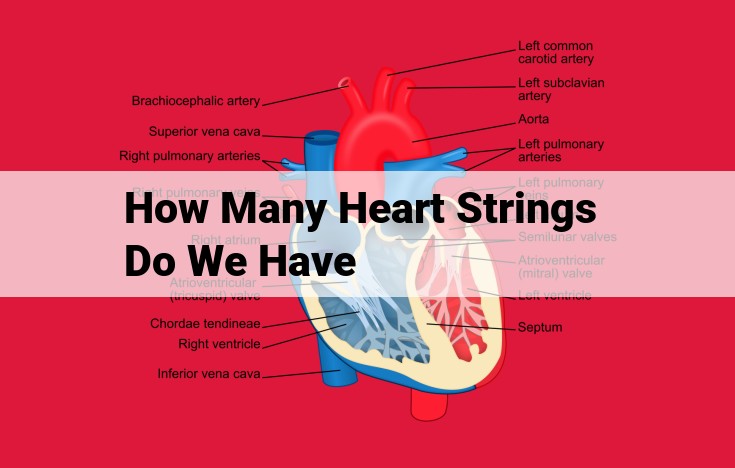
The heart is composed of anatomical structures that ensure proper blood flow. Atrioventricular (mitral and tricuspid) valves prevent backflow from ventricles to atria, while semilunar (aortic and pulmonary) valves prevent backflow from arteries to ventricles. Papillary muscles and chordae tendineae support these valves. The myocardium, the muscular layer of the heart, contracts to pump blood. The endocardium lines the heart chambers and valves. External entities aid in the assessment and treatment of heart conditions: electrocardiograms monitor electrical activity, echocardiograms visualize heart structures, cardiac catheterization diagnoses and treats issues, and cardiac surgeons and cardiologists specialize in heart care.
Dive into the Heart’s Guardians: Understanding Heart Valves
Your heart, the tireless engine of life, relies on a complex system of valves to ensure its rhythmic pump. These valves, like vigilant gatekeepers, orchestrate the smooth flow of blood, preventing backflow and maintaining the delicate balance of your cardiovascular system.
Atrioventricular Valves: Mitral and Tricuspid
As blood fills your heart’s atria (upper chambers), the mitral valve, also known as the bicuspid valve, guards the opening between the left atrium and left ventricle. Similarly, the tricuspid valve stands sentinel between the right atrium and right ventricle. These valves, anchored by flexible fibrous cords called chordae tendineae, swing open as the atria contract, allowing blood to enter the ventricles.
Semilunar Valves: Aortic and Pulmonary
When the ventricles contract, the aortic valve protects the opening between the left ventricle and aorta, the body’s main artery. Its three cusps prevent backflow of blood into the ventricle. Similarly, the pulmonary valve safeguards the exit from the right ventricle to the pulmonary artery, ensuring blood is pumped into the lungs for oxygenation.
Papillary Muscles and Chordae Tendineae: The Dynamic Duo
Papillary muscles, muscular projections within the ventricles, contract to create tension on the chordae tendineae. This tension closes the atrioventricular valves, preventing regurgitation (backflow) of blood into the atria.
Myocardium and Endocardium: The Heart’s Fabric
The myocardium, the thick muscular layer of the heart, is the driving force behind its contraction. The endocardium, a thin membrane lining the heart’s chambers and valves, protects them from damage.
Atrioventricular valves: Mitral and tricuspid valves
Anatomical Entities
Atrioventricular Valves: Guardians of the Heart’s Chambers
Within the intricate chambers of the heart reside two essential valves: the mitral and tricuspid valves. These guardians prevent the backflow of blood as it travels through the heart’s circuit.
Mitral Valve
The mitral valve, also known as the bicuspid valve, sits between the left atrium and left ventricle. It consists of two thin flaps, or cusps, that open and close with each heartbeat. When the left ventricle contracts, the cusps close tightly, preventing blood from flowing back into the atrium. Papillary muscles and chordae tendineae, fibrous cords that attach to the cusps, ensure their proper function.
Tricuspid Valve
The tricuspid valve, as its name suggests, has three cusps. It guards the passageway between the right atrium and right ventricle. Like the mitral valve, it opens during ventricular relaxation, allowing blood to flow into the ventricle, and closes when the ventricle contracts, preventing backflow into the atrium.
Papillary Muscles and Chordae Tendineae
Papillary muscles, located within the ventricle walls, are connected to the valve cusps by the chordae tendineae. These muscles contract during ventricular contraction, pulling the cusps closed and preventing regurgitation (blood leaking back into the atria).
Delving into the Heart’s Semilunar Valves: Aortic and Pulmonary
Our hearts, the tireless engines of life, pump life-sustaining blood throughout our bodies. Within these remarkable organs reside semilunar valves, the unsung heroes ensuring the blood’s unidirectional flow. Let’s unravel the intricate anatomy and functions of these crucial heart valves.
Aortic Valve: The Gatekeeper of Life
The aortic valve stands sentinel at the outlet of the left ventricle, the heart’s most powerful chamber. This three-cusped valve opens to allow oxygenated blood to surge into the aorta, the largest artery in our body. As the ventricle contracts, the valve snaps shut, preventing backflow into the heart. This synchronized motion ensures a constant supply of oxygen to our tissues and organs.
Pulmonary Valve: Guiding Blood to the Lungs
Mirroring the aortic valve, the pulmonary valve resides at the exit of the right ventricle. As the ventricle pumps deoxygenated blood towards the lungs, the pulmonary valve consisting of three cusps swings open. Once the blood is expelled, the valve closes tightly, preventing it from flowing back into the heart. This delicate mechanism ensures that deoxygenated blood travels to the lungs for purification and oxygenation.
Importance of Papillary Muscles and Chordae Tendineae
These valves do not operate in isolation. They rely on the support of two vital structures: papillary muscles and chordae tendineae. Papillary muscles, tiny muscular projections within the ventricles, are connected to the valve cusps by chordae tendineae, thread-like tendons. When the ventricles contract, the papillary muscles tighten the chordae tendineae, preventing the valves from bulging or prolapsing. This precise coordination ensures the valves remain closed, preventing blood from leaking back into the heart.
Clinical Significance: ECG, Echocardiogram, and Cardiac Interventions
Understanding the heart’s valves is crucial in diagnosing and treating heart conditions. Electrocardiograms (ECGs), utilizing electrodes placed on the body, provide electrical recordings of the heart’s activity, revealing abnormalities in valve function. Echocardiograms, employing ultrasound waves, offer real-time images of the heart, allowing physicians to visualize valve structure and motion.
For more complex valve issues, cardiac catheterization may be necessary. This procedure involves threading a thin catheter into the heart to diagnose and treat valve abnormalities. Skilled cardiac surgeons and cardiologists play pivotal roles in these interventions, repairing or replacing damaged valves, restoring the heart’s rhythm and function, and ultimately safeguarding our very lives.
The Heart’s Delicate Gatekeepers: Papillary Muscles and Chordae Tendineae
1. Anatomical Entities
The heart’s valves are crucial for directing blood flow and preventing backflow. Among these guardians are the atrioventricular valves, namely the mitral and tricuspid valves, which separate the atria from the ventricles. These valves are assisted by the semilunar valves, aortic and pulmonary valves, which guard the exits from the ventricles.
The Role of Papillary Muscles and Chordae Tendineae
Papillary muscles, small muscular protrusions within the ventricles, play a pivotal role in valve function. They act as anchor points for the chordae tendineae, fibrous cords that connect the valve leaflets to the papillary muscles.
When the ventricles contract, the intraventricular pressure rises. This pressure forces the valve leaflets to bulge into the atria. However, the chordae tendineae, under tension, prevent the leaflets from being pushed too far, ensuring that they do not prolapse back into the ventricles.
In this delicate ballet of cardiac mechanics, the papillary muscles and chordae tendineae work in concert to maintain valve competency. They prevent regurgitation – the backward flow of blood into the chambers – and ensure that blood is propelled efficiently through the heart’s chambers.
Other Related Entities
Electrocardiogram (ECG): This non-invasive test measures the heart’s electrical activity, providing insights into its rhythm and function.
Echocardiogram: An ultrasound technique that visualizes the heart’s structures and function, including the valves, offering valuable diagnostic information.
Cardiac Catheterization: An invasive procedure that involves threading a catheter into the heart to measure pressures, diagnose blockages, and potentially perform treatments.
Cardiac Surgeons and Cardiologists: These healthcare professionals specialize in the diagnosis and treatment of heart conditions, including valve disorders.
Describe the myocardium and endocardium
Understanding the Heart: Anatomical Entities and Related Entities
The human heart is a complex and vital organ, responsible for pumping blood throughout the body. To grasp its intricate workings, let’s delve into the anatomical entities and related entities that contribute to its functionality.
Anatomical Entities
1. Valves
The heart contains four valves that regulate blood flow:
- Atrioventricular Valves: The mitral valve and tricuspid valve prevent blood from flowing back into the atria during ventricular contraction.
- Semilunar Valves: The aortic valve and pulmonary valve prevent blood from flowing back into the ventricles from the aorta and pulmonary artery, respectively.
2. Papillary Muscles and Chordae Tendineae
Papillary muscles, tiny muscles within the ventricles, connect to the valves by thin, fibrous cords called chordae tendineae. When the heart contracts, these structures prevent the valves from being pushed back into the atria, ensuring proper blood flow.
3. Myocardium and Endocardium
The myocardium is the muscular layer of the heart responsible for contraction. Its coordinated contractions pump blood out of the heart. The endocardium is the innermost lining of the heart, protecting its chambers and valves from damage.
Other Related Entities
1. Electrocardiogram (ECG)
An ECG records the electrical activity of the heart. It can detect abnormal heart rhythms and provide insights into heart function.
2. Echocardiogram
Echocardiography uses ultrasound waves to create images of the heart. It allows doctors to visualize heart structures, measure their function, and detect abnormalities.
3. Cardiac Catheterization
This procedure involves inserting a thin catheter into the heart to diagnose and treat heart conditions. It can assess blood pressure, flow, and visualize blood vessels.
4. Cardiac Surgeons and Cardiologists
Cardiac surgeons perform surgery to repair or replace damaged heart valves, arteries, or other heart structures. Cardiologists diagnose and treat heart diseases non-surgically using medications, lifestyle modifications, and medical devices.
Electrocardiogram (ECG): A Window into Heart Health
Have you ever wondered how doctors can tell if our hearts are healthy with just a couple of electrodes attached to our skin? The answer lies in the electrocardiogram (ECG), a simple yet powerful tool that captures the electrical impulses that orchestrate our heart’s rhythm.
Imagine your heart as a symphony, where each note represents an electrical impulse. The ECG captures these notes, translating them into a graph that looks like a series of peaks and valleys. These deflections correspond to specific electrical events within the heart:
- The P wave indicates the electrical impulse that triggers the atria (the heart’s upper chambers) to contract.
- The QRS complex reflects the depolarization (electrical stimulation) of the ventricles (the heart’s lower chambers).
- The T wave represents the repolarization (recovery after depolarization) of the ventricles.
By analyzing the timing and shape of these deflections, doctors can assess various aspects of heart function:
- Heart rate: The ECG records the number of beats per minute.
- Rhythm: It helps identify abnormal heartbeats or arrhythmias.
- Cardiac conduction: The ECG can detect delays or blockages in the electrical pathway.
- Ischemia and infarction: Changes in the ECG can indicate areas of the heart that are not receiving enough blood or have suffered a heart attack.
Echocardiography: Unveiling the Secrets of Your Heart
In the realm of cardiology, echocardiography stands as an indispensable tool, providing a window into the intricate workings of the heart. Armed with sound waves, this non-invasive procedure offers invaluable insights into the heart’s structure and function.
Echocardiography begins with the deft placement of a transducer on the patient’s chest. This device emits high-frequency sound waves that travel through the body, bouncing off heart structures and creating images. These images can reveal a wealth of information about the heart’s anatomy, including the thickness and motion of the heart walls, the size and shape of the chambers, and the function of the valves.
By capturing these images in real-time, echocardiography enables physicians to dynamically assess the heart’s performance. It can detect abnormalities in valve function, such as regurgitation or stenosis, which may indicate underlying heart conditions. Additionally, it can identify structural defects, such as holes in the heart or enlarged chambers, providing crucial information for diagnosis and treatment planning.
Furthermore, echocardiography can assess the heart’s ability to pump blood effectively. By measuring the size and shape of the heart chambers, physicians can estimate the heart’s ejection fraction, which is the percentage of blood ejected from the heart with each beat. This measurement is vital for evaluating the heart’s overall health and function.
In conclusion, echocardiography is a powerful tool that allows cardiologists to visualize and assess the heart in a non-invasive manner. By providing detailed images and functional data, it plays a critical role in diagnosing and managing a wide range of heart conditions, ultimately improving patient outcomes.
Cardiac Catheterization: A Journey into the Heart
Imagine being a tiny explorer, embarking on an extraordinary journey through the intricate labyrinth of your heart. Cardiac catheterization is a minimally invasive procedure that allows doctors to navigate this vital organ, diagnosing and treating heart conditions without the need for open-heart surgery.
Through a small incision in your groin or arm, a thin, flexible tube called a catheter is inserted into a blood vessel. Guided by real-time X-ray imaging, the catheter is carefully threaded through your circulatory system until it reaches the target areas in your heart.
Investigating Heart Health
Cardiac catheterization serves as a powerful tool for assessing heart function. By injecting a special dye into your arteries, doctors can visualize blood flow patterns. This provides detailed insights into the structure and function of your heart valves, coronary arteries, and chambers.
If blockages or narrowing occur in your coronary arteries, cardiac catheterization enables doctors to perform balloon angioplasty or stent placement. These techniques help improve blood flow and reduce the risk of heart attacks. In some cases, cardiac catheterization can also be used to repair or replace damaged heart valves.
A Collaborative Effort
Cardiac catheterization is performed by cardiologists, medical specialists who diagnose and treat heart conditions. They may collaborate with cardiac surgeons, who perform more complex surgical procedures on the heart.
Importance of Advanced Imaging
To ensure accurate diagnosis and treatment, cardiac catheterization relies heavily on advanced imaging techniques such as echocardiography. Echocardiography uses sound waves to create detailed images of your heart’s structure and function, complementing the information obtained from cardiac catheterization. Together, these tools provide a comprehensive understanding of your heart’s health, enabling doctors to make informed decisions about your treatment.
The Heart: A Complex Symphony of Valves, Muscles, and Electrical Signals
1. Anatomical Entities
-
Valves:
- Atrioventricular Valves: Mitral (left) and tricuspid (right) – Control blood flow from atria to ventricles.
- Semilunar Valves: Aortic (left) and pulmonary (right) – Prevent backflow from ventricles into arteries.
-
Muscles:
- Papillary Muscles: Prevent valve leaflets from prolapsing into atria.
- Chordae Tendineae: Delicate fibers that attach papillary muscles to valve leaflets.
- Myocardium: The muscular wall of the heart that contracts to pump blood.
- Endocardium: The thin, inner lining of the heart that prevents blood leakage.
2. Other Related Entities
-
Electrocardiogram (ECG): A non-invasive test that measures the electrical activity of the heart, revealing heart rate, rhythm, and potential abnormalities.
-
Echocardiogram: An ultrasound-based imaging technique that visualizes heart structures in real time, showing valve function, chamber size, and any abnormalities.
-
Cardiac Catheterization: An invasive procedure that involves threading a catheter through an artery into the heart to inject dye for imaging or to perform interventional procedures.
Cardiac Surgeons and Cardiologists: Guardians of the Heart
The medical world relies on the expertise of both cardiac surgeons and cardiologists to diagnose and treat heart diseases.
Cardiac surgeons perform complex operations on the heart and its major vessels. They repair or replace damaged valves, bypass blocked arteries, and perform heart transplants. Their surgical skills and precision ensure the restoration of normal heart function.
Cardiologists, on the other hand, specialize in the non-surgical management of heart diseases. They use various diagnostic tests, including ECGs, echocardiograms, and stress tests, to identify and assess heart conditions. Additionally, cardiologists prescribe medications, recommend lifestyle changes, and provide guidance on preventive measures to optimize heart health.
Together, these dedicated professionals work as a team, collaborating to provide comprehensive care for patients with heart conditions. Their expertise and collaboration ensure that every heart has the best chance to function optimally for a healthier and more fulfilling life.